Talk to an expert : +1 (305) 874-0316
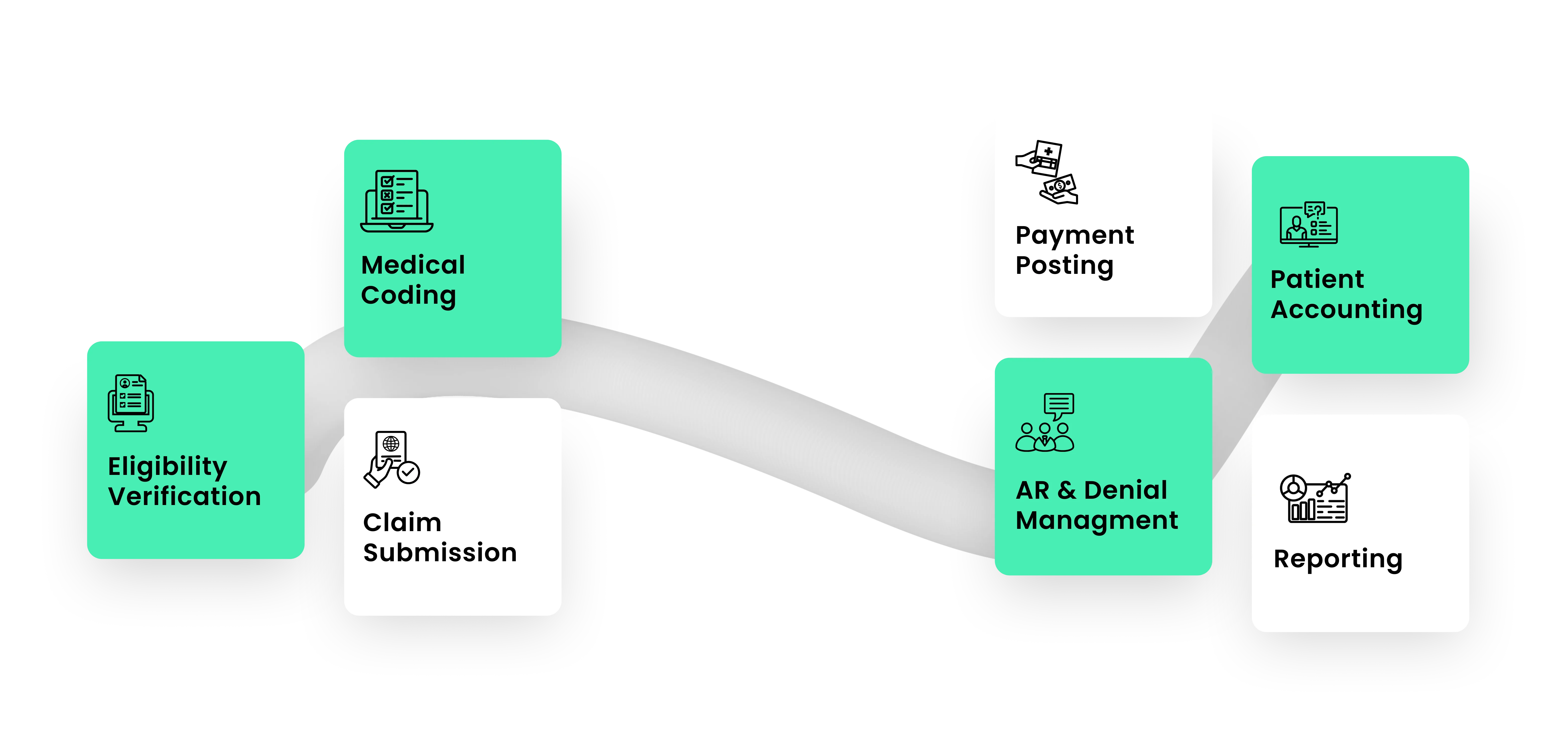
At Fresh RCM, we are dedicated to transforming the financial health of dermatology practices through expert Revenue Cycle Management services. Our team comprises seasoned professionals with extensive experience in dermatology billing and coding, committed to delivering excellence in every aspect of RCM.
Top Dermatology Medical Billing & RCM Services in Florida